ICSI Treatment in Chennai: Success Rates, Cost & When It’s Recommended
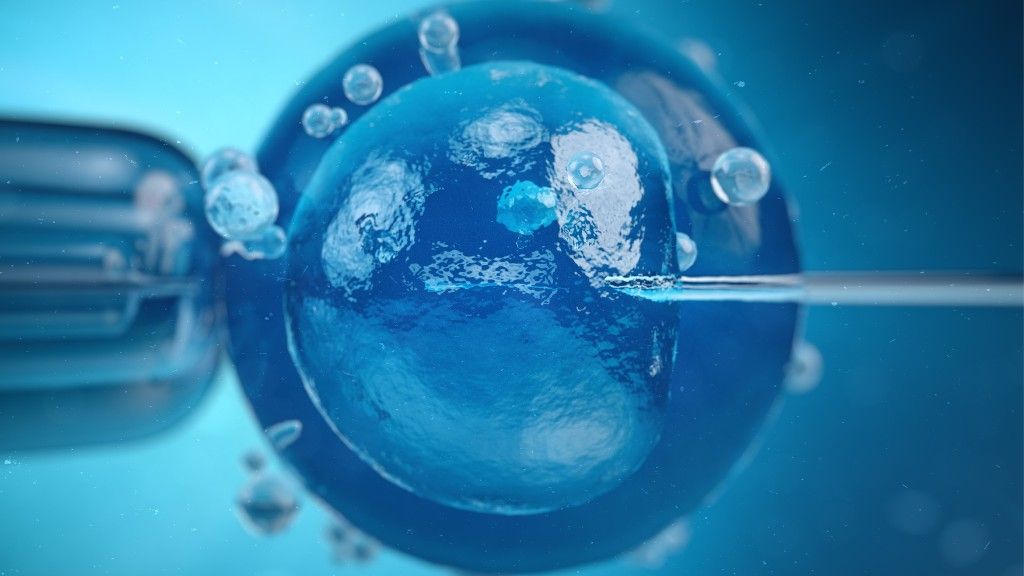
ICSI Treatment in Chennai: Success Rates, Cost & When It’s Recommended Home ICSI February 15, 2026 Introduction When you’ve been told that male factor infertility or previous fertilization challenges might require ICSI treatment in Chennai, you probably have questions about what this procedure involves, how it differs from standard IVF, and whether it’s the right choice for your situation. ICSI—Intracytoplasmic Sperm Injection—represents a significant advancement in assisted reproductive technology, offering hope to couples who might not achieve fertilization through conventional IVF methods. Understanding when ICSI is recommended, what success rates you can realistically expect, and how to navigate the financial and emotional aspects of this specialized treatment empowers you to make informed decisions. This comprehensive guide explains everything you need to know about ICSI, from the science behind the procedure to practical considerations for couples in Chennai seeking this advanced fertility solution. What Is ICSI? Understanding the Procedure ICSI is a specialized laboratory technique used during IVF where a single sperm is directly injected into an egg using microsurgical equipment. Unlike conventional IVF, where thousands of sperm are placed around each egg and fertilization happens naturally in the laboratory dish, ICSI involves the embryologist selecting one sperm and precisely injecting it into the egg’s cytoplasm. The Science Behind ICSI The procedure requires highly skilled embryologists working with sophisticated micromanipulation equipment under powerful microscopes. After egg retrieval, each mature egg is prepared by removing the surrounding cells. The embryologist then selects the healthiest-appearing sperm, immobilizes it, and carefully injects it through the egg’s outer layer directly into the center. This bypasses the natural barriers that sperm must normally overcome to fertilize an egg. Following injection, the eggs are placed in specialized incubators where fertilization is monitored over the next 16-18 hours. Successfully fertilized eggs develop into embryos that are cultured for several days before transfer to the uterus, just like in conventional IVF. ICSI vs IVF Chennai: Understanding the Difference Many couples wonder about ICSI vs IVF in Chennai and which approach their doctor will recommend. The fundamental difference lies in how fertilization occurs. Conventional IVF: Eggs and sperm are combined in a culture dish, and fertilization happens naturally when sperm penetrate the eggs on their own. This approach works well when sperm quality and quantity are normal. ICSI: The embryologist actively injects a single sperm into each egg, completely bypassing the natural fertilization process. This technique overcomes barriers that prevent sperm from fertilizing eggs independently. The rest of the IVF process—ovarian stimulation, egg retrieval, embryo culture, and embryo transfer—remains identical whether conventional IVF or ICSI is used for fertilization. When Is ICSI Recommended Over IVF? Understanding when is ICSI recommended over IVF helps you comprehend why your fertility specialist might suggest this approach for your specific situation. Male Factor Infertility Indications Severe Oligospermia: When sperm count is extremely low, there aren’t enough sperm for conventional IVF to work effectively. Poor Sperm Motility: If sperm cannot swim properly, they cannot reach and penetrate eggs even in the controlled laboratory environment. Abnormal Sperm Morphology: When the majority of sperm have structural abnormalities, they may be unable to fertilize eggs naturally. Obstructive Azoospermia: When sperm production is normal but blockages prevent sperm from reaching the ejaculate, surgical sperm retrieval combined with ICSI enables fertilization. Non-Obstructive Azoospermia: Even when very few sperm are produced, surgical extraction followed by ICSI can sometimes achieve fertilization. Previous Vasectomy: For men who’ve had vasectomies, sperm can be surgically retrieved and used with ICSI regardless of whether vasectomy reversal is possible. Previous Fertilization Failure If conventional IVF resulted in poor or failed fertilization despite apparently normal sperm parameters, ICSI is typically recommended for subsequent cycles. Sometimes fertilization problems exist that aren’t detected by standard semen analysis. Limited Egg Numbers When ovarian response produces only a small number of eggs, ICSI maximizes the chance that available eggs will fertilize, rather than risking complete fertilization failure with conventional methods. Use of Frozen or Surgically Retrieved Sperm Sperm that has been frozen or surgically extracted typically works better with ICSI than conventional IVF, as these sperm may have reduced fertilization capacity. Preimplantation Genetic Testing (PGT) When embryos will undergo genetic testing, ICSI is often preferred because it eliminates the possibility of contaminating DNA from excess sperm cells affecting test results. Unexplained Infertility In some cases where infertility causes remain unclear, ICSI may be recommended to ensure fertilization occurs, particularly if there’s concern about potential fertilization problems. ICSI Success Rate Chennai: What to Expect Understanding ICSI success rate in Chennai requires context about the factors that influence outcomes. Realistic Success Expectations ICSI fertilization rates typically range from 60-80%, meaning this percentage of mature eggs injected usually fertilize successfully. However, fertilization is just the first step. Not all fertilized eggs develop into viable embryos, and not all embryo transfers result in pregnancy. Overall pregnancy rates with ICSI depend significantly on maternal age, egg quality, embryo quality, endometrial receptivity, and underlying fertility diagnoses. For women under 35, pregnancy rates per transfer typically range from 40-50%, while women over 40 may see rates between 15-25%. Factors Affecting ICSI Outcomes Maternal Age: Egg quality declines with age, impacting embryo development regardless of fertilization method. Sperm Quality: While ICSI overcomes many male factor issues, extremely poor sperm DNA quality can still affect embryo development. Egg Quality: The procedure cannot improve egg quality, which remains the most significant factor in successful embryo development. Embryologist Expertise: ICSI requires exceptional technical skill. Experienced embryologists achieve better fertilization rates with minimal egg damage. Laboratory Conditions: Optimal culture conditions, equipment quality, and quality control protocols significantly impact outcomes. ICSI vs Conventional IVF Success Rates When ICSI is appropriately indicated, success rates are comparable to or better than conventional IVF for that specific couple. However, for couples without male factor infertility or other indications, conventional IVF and ICSI show similar overall success rates. The key is using the right technique for the right situation. ICSI Cost in Chennai: Financial Considerations Understanding ICSI treatment cost in Chennai Tamil Nadu